Brachial plexus birth palsy is an injury to the nerves of brachial plexus (C5-T1) during the process of delivery. This palsy occurs in 1 to 3 children out of 1000 live births. This injury may affect the entire brachial plexus or its upper or lower divisions [Upper brachial plexus (C5-C6) and lower brachial plexus (C7-C8-T1)].
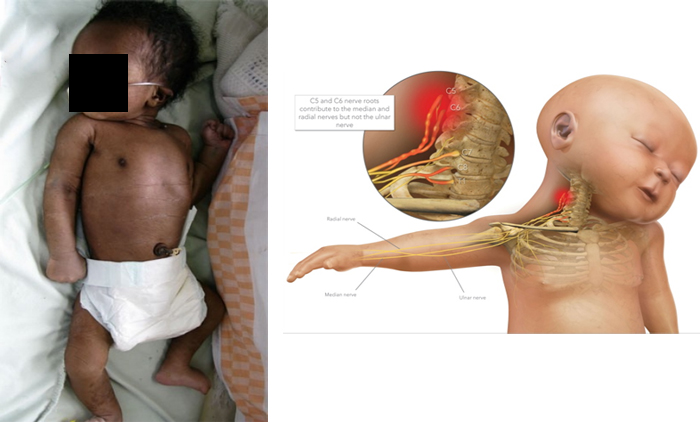
During difficult delivery the nerve gets stretched, compressed or torn leading to weakness or paralysis of the muscles of arm, elbow and hand.
Many children with brachial plexus palsy recover on their own. But if the condition does not completely resolve within 1 month, it usually has lasting effects. That’s why we encourage you to have your child assessed 1 month after their birth if they have not fully recovered. If treatment is needed, it is important to begin early.
In cases of mild injury(neurapraxia), majority of children recover full function by 6-8months. However children with moderate to severe stretch (leading to neurotmesis or axonotmesis), usually don’t recover fully and need physiotherapy/electrical stimulation.
Physiotherapy is usually started after 6 weeks of birth but we should start passive range of exercises as soon as possible after birth to gain muscle strength and to prevent contractures.
Neuromuscular electrical stimulation used as a rehabilitation adjunct to promote nerve regeneration following brachial plexus injury. It enhances muscle activation in a weak or poorly innervated muscle group. It also helps in inhibition of muscle atrophy during the period of re-innervation.
It is a therapeutic current which has no side effects and is given by the calibrated electrical stimulation machine.

Physiotherapy is the most recommended form of treatment for minor to moderate cases. Children With neurapraxia recover completely in 6-8 weeks so we teach home based exercise to their parents. However children with axonotmesis and neurotmesis do not recover completely with home based exercises and so physiotherapy plays a vital role for their recovery. If these children do not get physiotherapy at the right time, they may develop contractures and muscular weakness leading to permanent disability of the affected limb.
Children with panplexpathy(flaccid limb) with no progressive improvement on physiotherapy and electrical stimulation need nerve reconstruction surgeries.
Many specialists (Paediatric orthopedic, Paediatric Neuro, Physiotherapist, Occupational therapist and orthotist) are required to be involved in care of children affected from BPBP. Team of doctors with passion to treat this condition, joined their hands to optimally address issues related to BPBP. Parents get a consolidated comprehensive opinion about their child without the need of visiting different centers. All the consultants assess and advice under one roof, making it very convenient for parents.
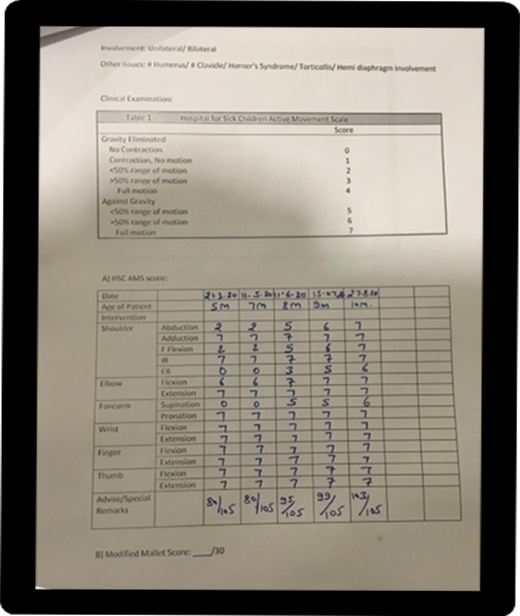
Gross improvement can be observed by the family. However detailed and precise improvement can be assessed by charting all the movements of affected upper limb over a active movement scale. We use Hospital for Sick Children Active Movement Scale (HSCAMS) for assessing movements.